Discount naprosyn 250 mg on line
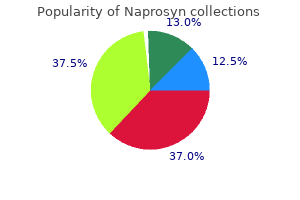
This allows for maximum rigidity of the construct so that some weight bearing can be initiated immediately postoperatively. If laboratory values are elevated or suspicious for infection, a fluoroscopic guided aspiration should be perfromed and sent for cell count, Gram stain, and cultures to rule out infection. Small rings are more rigid than large rings, but smaller rings may hinder skin care and may cause soft tissue compression if there is postoperative swelling. A peripherally inserted central catheter is used if intravenous antibiotics will be given for several weeks. The patient is in the left lateral decubitus position: proximal to the right and distal to the left. The environment of the injury has special significance for open fracture management. Galeazzi procedure the hamstring tendon is passed retrograde through the patellar tunnel using a Huysten suture passer or a guide pin with an eyelet. Postoperatively, the pins are cleaned daily with saline and redressed with a Kerlix dressing wrapped tightly around each set of pins. It is passed first under the patellar tendon and then through a medial capsular tunnel. The ulnar nerve courses through the cubital tunnel posterior to the medial epicondyle. The posterior approach is the most commonly used route for spinal fusion and instrumentation in the scoliotic spine. Ultrasounds of dislocated right hip with alpha angle of 56 degrees (A) and normal left hip with alpha angle 66 degrees (B). The solid arrow shows the intact cartilage side and the open arrow shows the osteochondritis dissecans side. The medial screw is easily directed posterolaterally and the lateral screw posteromedially. Proximally, the gluteus maximus muscle is detached from the gluteus medius almost up to the iliac crest, but the skin incision does not necessarily extend so far proximally. No genetic defect has been identified, and no common teratogen is linked to fibular deficiency. The exact placement of the retractor is outside the labrum and inside the capsule. The deformity is usually correctable at first and then progresses to a fixed deformity as myostatic contracture develops. Partial injuries (sprains) occur as a result of lower energy and are more common with axial load and plantarflexion, such as in competitive sports. The surgeon should not hesitate to perform this procedure before 1 year of age in resistant cases (9 to 12 months). Attention is turned to the medial wall, where the superomedial fragment is identified. Placement in this location with the knee flexed also minimizes the risk of injury to the posterior vascular structures. Valuable information regarding alignment and limb-length discrepancy is determined by using these films. This delay between resection and reimplantation allows the surgeon to monitor the patient and assess for possible recurrence after the antibiotics have been stopped. One-stage correction of the spastic dislocated hip: use of pericapsular acetabuloplasty to improve coverage. The family should be informed if there is growth plate damage before the treatment. When performing the medial parapatellar skin incision, care should be taken to avoid inadvertent transection of the infrapatellar branch of the saphenous nerve; if a branch is cut it should be buried in fat to decrease the risk of developing a neuroma. Slightly incomplete coverage of the acetabular component (up to 20%) may be acceptable. Temporary use of an external fixator (one or two pins proximally and one or two pins distally) with the pins placed out of the path of the nail will hold the fusion in a compressed and properly rotated position when inserting the rod. In general, the higher the level of the defect, the higher the prevalence of scoliosis. The patient is assessed every 2 weeks in the outpatient clinic with radiographic and clinical examinations.
Purchase naprosyn online pills
All half-pins must be placed into safe zones of the leg to avoid inadvertent neurovascular injury. Attention to spinal cord monitoring is crucial at this point in the operation to avoid undue neurologic injury. All patients should have the appropriate infection laboratory studies (ie, complete blood count, C-reactive protein, erythrocyte sedimentation rate) as well as an attempt at knee aspiration and synovial fluid sent for Gram stain, cell count, and culture. On the second and third postoperative days, the patient transfers to and from the bed and chair, sits up in a chair, and ambulates with weight bearing as tolerated using a walker or crutches. When using the drill, it is imperative that the drill bit not heat up and cause osteonecrosis of the bone. For patients with external fixation, once the bone has consolidated, the frame is then dynamized in the office 1 month before removal. The rectus femoris muscle is separated from the other muscles of the quadriceps muscle group proximally (arrow). Once exposure is obtained the interposed periosteum can be removed by using a Freer elevator to carefully sweep this periosteum out of the physis. An image intensifier is useful for accurate localization of the lesion, during percutaneous procedures, and for intraoperative confirmation that the entire lesion is being addressed. It is commonly difficult to distinguish between a medial collateral ligament tear, a meniscal tear, or an acute patellofemoral subluxation or dislocation. Interdigitated skin flaps are similarly reapproximated with multiple interrupted 5-0 absorbable suture. Diminished knee flexion after hamstring surgery in cerebral palsy: prevalence and severity. The outer cortex of the graft should be buried below the outer cortex of the ilium. This can best be accomplished by determining the rod length to be used preoperatively from an erect lower limbs radiograph. Optimal cement fixation of the acetabular component is difficult to achieve without a dry surgical field, making hypotensive anesthesia a crucial aspect of cement technique. Communication between the monitoring and anesthesia teams should be facilitated to prevent any change in neurologic function brought on by anesthetics, hypotension, or low blood volume. The extremity is carefully cleaned and draped to allow adequate exposure for the surgical approach to the medial hamstring muscles. It affords complete access to the posterior capsule to perform a capsulectomy and remove any retained osteophytes from the previous surgical procedure. Casts applied too tightly or not appropriately split can lead to acute compartment syndrome. Low-profile plates may help avoid irritation from the plate before fracture healing. If the remnant of the discoid meniscus is unstable or torn, requiring fixation or stabilization, a posterolateral approach should be made for inside-out suture fixation. Stretching and strengthening programs, along with active functional use activities, are carried out by the therapist as well as taught to the parents and child as a home program. A "perfect cement technique" should be avoided, since this can make removal, at the time of reimplantation, more difficult. For the ambulatory patient, observation of gait may show hyperlordosis, limited step length, scissoring gait, or crouch gait. Reconstruction of a ruptured patellar tendon with Achilles tendon allograft following total knee arthroplasty. The first titanium marker has been placed centrally within the metaphysis proximal to the physis. When examining a child for hip flexion contracture, the examiner should not be misled by the presence of a knee flexion contracture that prevents full extension of the leg. A Grammont procedure4 is performed to medially transfer the patellar tendon if patellar maltracking is significant. Open reduction and internal fixation for supracondylar humerus fractures in children.

Cheap 250 mg naprosyn with amex
The medial and lateral inferior genicular arteries arise from the popliteal artery and pass deep to the collateral ligaments to supply the medial and posterolateral periosteum of the proximal tibia. The use of pulsatile lavage can reduce that risk by removing fat and marrow from the femoral canal. Pedicle width decreases from T1 to T4 and then gradually increases to T12, while pedicle height and length tend to increase from T1 to T12. It can be fixated with either a mini-fragment plate that bridges from the posterior facet to the anterolateral fragment, or a lag screw from the anterolateral fragment to the superomedial fragment. With the Roux-Goldthwaite procedure, there are reports of patellar tendon rupture of the untransferred tendon. Knee is positioned in full extension, and the new position for the patella is marked on the synovium. Patient education is important to maximize understanding of wound risks and compliance with elevation and other postoperative treatments. Experimental epiphysiodesis: magnetic resonance imaging evaluation with histopathologic correlation. The leg can be placed supine on the operating table, with the hip flexed and the knee flexed 90 degrees. Distal osteotomy is parallel to chisel; proximal osteotomy is perpendicular to shaft. Note the 90-degree-flexed position of the elbow and the 90-degree external rotation of the shoulder. Sublaminar wires also offer an attractive option and are useful if lateral translation of the spine is required. If significant spasticity is present, pain and spasm may lead to difficulty in maintaining postoperative positioning in extension and abduction, leading to recurrence of hip flexion or adduction contractures. Thumb muscle involvement, motion, and stability should be evaluated in the physical examination before organizing the treatment plan. After pin removal, the patients are instructed to begin gentle active-assisted shoulder range of motion. The femoral component obtains intial fixation through a press-fit in either the metaphysis or diaphysis and has a surface that allows for in- or on-growth of bone. This sizing tray is a jig for drilling final fixation holes for the tibial component and determines its ultimate mediolateral, anteroposterior, and rotational position. With a cemented knee, full weight bearing under the supervision of a therapist is allowed on the first or second postoperative day. The majority of supracondylar fractures of the humerus (other than extension type I fractures) are unstable; therefore, stabilization in the form of cast immobilization or preferably operative fixation is usually necessary. Neurologic injury the risk of neurologic complication increases with the amount of reduction performed. The one that is commercially available is called the Wichita Fusion Nail (Stryker). There is a significant amount of hematoma formation and torn periosteum; thus, the incision length allows the surgeon to define the appropriate anatomy and prepare the fragment for reduction. A thorough physical examination should include: Observation of the lower extremity. We would prefer to perform physeal bar resection alone first, then correct any residual angular deformity when physeal growth is complete. Treatment of subluxation and dislocation of the patella in the child: Elmslie technic with movable soft tissue pedicle (8 year review) [in German]. The angle between the shaft and the neck is approximately 125 degrees, with 15 degrees of anteversion related to the posterior femoral condyles. If difficulty is encountered while placing screws at L5, the surgeon can wait until the decompression is done and then use a Woodson elevator to palpate the pedicle within the canal. It may occur because of the decreased size of the nasopharynx resulting from anterior displacement of the atlas. The pain may decrease with weight bearing as the component reseats itself and motion at the bone implant interface decreases.
Naprosyn 250mg without a prescription
Functional impairment and pain are unusual complaints, except in the case of active triggering. Before making a skin incision, fluoroscopy is brought into the surgical field and the surgeon draws on the skin the physis location, the physeal bar location, the surgical approach trajectory, and the skin incision location that will permit the desired approach. The knee is immobilized for 3 days in 20 to 30 degrees of flexion in a Robert Jones dressing to avoid sciatic nerve stretch. An oscillating saw is used to perform the posterior portion of the osteotomy just superior to the linea aspera. To replace the distal femur, existing epicondyles are osteotomized, and the deficient distal femur is cut to expose viable, stable host bone. Stringent surveillance by medical oncologists for bony metastases must be encouraged, therefore, with early referral to the orthopedic surgeon before pathologic fractures occur. The femoral component is applied to the condyle and impacted with the punch held at 30 degrees to the long axis of the femur. Femoral preparation is difficult and may require traction, hip extension, and the use of a hook to deliver the femur anteriorly for preparation. Closure of the soft tissues over the plate: closure of the pes bursa (solid white line) over the distal portion of the plate to its anatomic location; closure of the incision in the sartorius fascia (square dotted line), just above the gracilis tendon; closure of the superior split in the retinaculum (dotted diamond yellow line), just medial to the patellar tendon. The table mattress padding under the thigh segments can be built up to keep the hips relatively extended. Computed tomography shows bone well and is most helpful to evaluate hip incongruity during the late stages of remodeling and during young adulthood. While nonoperative treatment yields the fewest iatrogenic complications, it accepts malunion in nearly 100% and a higher incidence of later subtalar fusion. The muscle belly is reflected distally off its proximal origin, allowing easy access to the lateral capsule of the talus. Approach All standard and minimally invasive approaches for exposure of the knee joint can be applied and supported with the navigation system. If the reduction is stable, as is usually the case, no internal fixation is required. A 6- to 8-week home or formal physical therapy program is instituted, incorporating range of motion, stretching, progressive strengthening, and functional or sport-specific training. Synovial white cell count differential may be of greater value, but data to recommend this routinely are limited. Extra cement is removed while pressure is maintained on the acetabular component using a Charnley pusher centrally to minimize angular forces on the cement mantle until the cement has hardened. The device works very well for the primary knee arthrodesis that has good metaphyseal bone. The involved limb is placed in neutral abduction, neutral rotation, and 0 degrees of extension. Flexion contractures are harder to address arthroscopically, but a posterior release can be performed using small, open, medial and lateral incisions. Percutaneous intramedullary fixation of long bone deformity in severe osteogenesis imperfecta. Operative treatment of displaced medial epicondyle fractures in children and adolescents. However, progression of the deformity with growth leads to increased soft tissue pressure, bursa formation, and risk of skin ulceration over the medial malleolus, lateral malleolus, or talonavicular region. Arterial thrombosis due to tourniquet application, arterial kinking during knee manipulation, and direct, sharp injury to the artery have been described. For proper assessment of the acetabular shape and version, the central x-ray beam must be centered about 2 cm above the symphysis pubis. One-stage revision surgery of the infected hip: A minimum 10-year follow-up study. Any perceived deformity or pain to palpation should trigger dedicated radiographs of the problematic region. Apparent leg length is measured with the patient supine with the legs parallel to each other.
Diseases
- Hemoglobinopathy
- Xeroderma pigmentosum, type 7
- Intractable singultus
- X chromosome, trisomy Xp3
- Palmoplantar Keratoderma
- Narrow oral fissure short stature cone shaped epiphyses
- Cerebral malformations hypertrichosis claw hands
Purchase naprosyn with paypal
Retractors placed over the anterior wall need to be placed directly on bone to avoid injury to the nerve. Approximately 10% have minor loss of extension (10 to 15 degrees) at 1 to 2 years. From 1987 to 2000, only the Ilizarov apparatus was used with fixation across the knee joint with a hinge. If more of the medial wall is cut, then the fulcrum of rotation will move posteriorly and more lateral coverage will be obtained. The acetabulum is then repositioned with internal rotation and some forward tilt extension. If the inner table has been exposed, this can be confirmed with direct visualization. Appropriate full-length forearm imaging must be performed at the end of the case to ensure an acceptable rotational relationship between the radial styloid and the bicipital tuberosity, as well as the ulnar styloid and the coronoid process. Blood loss may be minimized by sealing the epidural veins on the inner aspect of the hemivertebral wall and pedicle with a bipolar cautery before resecting these areas. Because of open growth plates, standard plate-fixation techniques are rarely indicated. If the patient has subluxated or dislocated the hip in a previous procedure, the external fixator should be extended above the hip with a hinge device similar to that used for the knee. Several interrupted absorbable sutures (typically 3-0 Vicryl) are used for closure of the subcutaneous and subcuticular portion of the radial wound. Extensive periosteal stripping of fracture fragments is avoided and fragments are carefully hinged on their soft tissue attachments to preserve their vascularity. Threaded K-wire spinous process fixation of the axis for the modified Gallie fusion in children and adolescents. Most prosthetic infections are treated with two-stage revision arthroplasty of the knee, in which either a static antibiotic spacer or a dynamic articulated type of spacer is used for the first stage of the revision. Increased pelvic incidence has been associated with increased shear forces and the development of spondylolisthesis. A one-and-a-half spica cast is used for infants and young children (less than 6 years) to minimize stress across the pseudarthrosis. Fracture reduction Difficult reduction is often secondary to soft tissue interposition. If a gentle concentric closed reduction is achieved and the patient is over 18 months old, a Salter innominate osteotomy including intramuscular psoas lengthening without open hip reduction can be performed. Compartment syndrome has been associated with this positioning for femoral shaft fracture treatment. If the hemivertebra is in the thoracic region, it will be necessary to resect the rib head first to obtain access. Bone loss Small contained bony defects can be addressed with either cement or morselized bone graft. Preoperative assessment of the hips is important to anticipate the intraoperative positioning, and if the flexion contractures about the hips are too severe, a preliminary release of contractures done a few weeks ahead of time may be necessary to allow for proper positioning of the legs at the time of the kyphectomy. Complications of the infection are failure to cure the infection and side effects or toxicity related to antibiotic use. Without moving the arm, the image can be rotated to obtain an axillary lateral view. An indwelling bladder catheter is used during the surgery, since much of the surgery is intrapelvic. Exact posterior facet reduction is difficult to achieve but required to achieve excellent results. At 6 weeks after the operation, strengthening exercises of the abductor muscles can be started. It allows for optimization of component alignment, size, and rotation, while providing the opportunity to restore the joint line.
Buy 500mg naprosyn with visa
Alternatively, the tendons can be left attached distally and an open tendon stripper used to release the tendons proximally. Tensile forces along the lateral border of the metatarsal result in a transverse fracture. Meticulous soft tissue handling helps the tissues to heal and minimizes postoperative complications. In most systems, femoral head reaming is performed by cannulated reamers that pass over the central guide pin. The extensor mechanism should be treated with care to avoid avulsion of the patella tendon insertion. Delay in surgical stabilization can lead to further meniscal and chondral injury due to recurrent instability. Access is via the interval between the flexor hallucis longus and the peroneal muscle belly. The posterior limb of the fascia lata graft is passed under the lateral collateral ligament. The underlying gracilis (superior) and semitendinosus (inferior) tendons are identified by palpation. This is the most functionally disabling deformity in hemiplegia as it significantly interferes with grasp and release function. Tibial rotation is determined by the surgeon using the appropriate tibial template and tracker. Avascular necrosis has not been demonstrated in children in whom this technique has been used. This can be done through the knee, reaming the tibia and femur separately, or from the hip using long 80cm reamers (Biomet Trauma, Stryker). It is recommended that these plans be recorded on a "blueprint" that can be placed on the operating room wall outlining the location of implants, osteotomies, and order of progression for the surgical plan. Once the prosthesis is assembled, a trial reduction is carried out and tested for stability. In the standing position, the entire weight of the upper body is transmitted through the hips to the lower extremities. Spinous process identified via palpation after dissection down to the thoracodorsal fascia. Reconstruction of severe acetabular bone-deficiency: the Burch-Schneider antiprotrusio cage in primary and revision total hip arthroplasty. The iliotibial band is incised slightly anterior to the line of the skin incision so that the fascial incision passes directly over the most prominent point of the trochanter and remains 5 to 10 mm anterior to the insertion of the gluteus maximus tendon into the proximal femur. A longitudinal incision is made in the joint capsule, along the femoral neck and transversely from the proximal femur. Malunion of fractures can occur with operative or nonoperative treatment or can be a secondary consequence of premature physeal closure. Gradually revascularization of the epiphysis begins, usually at the anterolateral area of the epiphysis. Articular cartilage Articular cartilage delamination along the anterior and superolateral acetabular rim is common. Interposed biceps tendon, interposed periosteum, and buttonholing of the shaft through the deltoid are possible causes of inability to obtain a reduction. Palpate along the joint line, medial and lateral collateral ligaments, iliotibial band, and pes anserine to identify any tenderness suggestive of focal injury. A consideration when performing the final fusion is that posterior osteotomies may be required, especially if a subfascial technique is employed, because the posterior elements may become stiff after repeated exposures. The pathoanatomy is individually specific and highly variable and may consist of a pure ligamentous injury, a pure bony injury (fracture), or a combination. Once the cortex has been entered the drill is angled obliquely to fashion a tract. With the trigastric flap approach there is no apophysis to repair, but the trigastric tendon has to be fixed to the cartilaginous trochanter. Procedure of choice: replacement arthroplasty the decision regarding bipolar versus total hip arthroplasty is a function of acetabular involvement, preexisting arthritis, and life expectancy.
Purchase naprosyn 250mg amex
The fascia overlying the (superficial) posterior compartment is divided and the underlying tendon is identified. Autograft is preferred, but soft tissue allograft could be considered based on patient preference. The distraction device is connected to the clamps, and final tightening is performed. Chapter 29 Surgical Repair of Irreducible Congenital Dislocation of the Knee Matthew B. The number of points to be acquired is shown in the center of an acquisition clock. Pending those findings, appropriate implant selection should be undertaken as well, whether to proceed with a tapered stem, a fully coated medullary-locking stem, or include a cemented stem. Stump closure with interrupted absorbable sutures after insertion of a Steinmann pin to stabilize the heel pad. By sliding the distal end of the guide mediolaterally at the ankle, a final adjustment can be made to centralize it over the center of the talus and to minimize the risk of varus inclination of the cut. When distal bone is severely deficient, total femoral replacement may be considered. This makes a strong case for provisional external fixation of reduced talus fractures as immediate treatment, particularly if the condition of soft tissues does not allow early open management. The gracilis muscle has a relatively small physiologic cross-sectional area and a relatively large ratio of tendon length to muscle fiber length, indicating that it is designed for maximal excursion and diminished force generation. The anatomic tibiofemoral angle is the angle between the midshaft lines of the femur and the tibia. Abnormalities in vertebral rotation become apparent as an asymmetrical rib hump, prominence, or fullness, leading to possible identification of patients at risk for having scoliosis. After 8 to 10 weeks, walking is allowed with a cane, which should be used until the abductors are strong enough to stabilize the hip. Lengthening may be performed by inserting the distractor between the rods through the slot of the tandem connector. Preoperative Planning Thorough preoperative planning is the key to a successful reconstruction. Fluoroscopic image showing the osteotomy wedge in place with the guide pins just superior to it. Most categorize the fractures based on amount of angulation,2 usually in 30-degree increments, while some also include translation. Additional concerns are bilateral extremity fractures and fractures at different stages of healing. If the anterior fascia of the thigh and the fascia of the sartorius muscle are tight, they are released. Based on modeling studies, the hamstrings are a significant contribution to increasing the force in spastic hip disease, which causes hip subluxation. Inappropriate lengthening of the lateral hamstring muscle may result in excessive weakness, resulting in a recurvatum gait pattern (characterized by rapid and excessive knee hyperextension in stance phase). The approach can be made slightly more medial or lateral depending on the location of the fracture. The peak in age distribution at age 2 is due to relative weakness of primarily woven bone at a time when ambulation increases the risk of fall-related trauma. Increasing the gap between the wires at the fracture site increases rotational control. Distal fibula fractures in skeletally immature patients may also be cross-pinned if the fracture pattern allows. Ideally, it is accomplished at one or two levels in a location that will leave sufficient midlumbar fixation points to push the vertebrae forward to create lordosis. Either of two types of connectors may be used: a tandem connector, which houses the cranial and caudal rods inside a rectangular box so the ends meet end to end, or side-to-side connectors, which allow the rods to overlap. These augments offer a custom reconstruction option that permits load-bearing and supports cement fixation. As the fang crosses the fracture site, proximal fragment intramedullary canal entry is often facilitated by nail rotation.
Purchase naprosyn without prescription
Malunion typically occurs in varus and usually occurs if malalignment is accepted or unrecognized or union is not achieved or fixation fails. During the 5th and 6th weeks of gestation, interdigital clefts form through the process of apoptosis, or programmed cell death, beginning at the digital tips and proceeding in a distalto-proximal direction. Trigger thumbs in children: a follow-up study of 37 children below 15 years of age. Healthy soft tissue must be present on both sides of this arc to allow effective repair during closure. Consider detaching or splitting along the anterior third of the gluteus medius to eliminate the risk of damage to the superior gluteal nerve, which passes 4. A Stulberg footrest or equivalent device is used to control knee flexion during surgery. Hemiresurfacing, in which only the femoral head is resurfaced, has largely been abandoned because it provided suboptimal results. The shaft is supplied by a single nutrient artery that enters from the medial cortex at the junction of the proximal and middle thirds of the diaphysis. A knee immobilizer sometimes may be worn by the patient until he or she can do straight leg raising without difficulty. Mechanical axis deviation of the lower limbs: preoperative planning of uniapical angular deformities of the tibia or femur. Better results were also seen with an anatomic reduction versus a nonanatomic one. Once the reduction is checked, the nails are passed across the fracture line and advanced until they reach their final endpoint. Does the patient complain of pain only, instability only, or pain plus instability This distinction is important in the multiply injured knee with chronic ligamentous deficiency and arthritic change. The goals for surgical intervention in the patient with metastatic carcinoma to bone are relief of pain; prevention of impending pathologic fracture; stabilization of true fractures; enhancement of mobility, function, and quality of life; and, for some, improved survival. The fracture boot should be worn during the night for the initial 3 to 4 weeks after surgery to prevent an early Achilles tendon contracture. If the lateral cortex has been breached, then either a staple or a 2- or 3-hole plate must be placed at the lateral cortex to restore stability to the lateral hinge. This is effective to treat crouch in the presence of a knee extension lag without knee flexion contracture. The correction phase begins with lengthening the leg by 7 to 8 mm at a rate of 1 mm per day (0. Some of these might be a complication of the treatment (poor reduction, open treatment, or internal fixation) rather than the natural history. For patients close to skeletal maturity, interfragmentary fixation can be used with or without a one-third tubular plate just as in a skeletally mature patient. Postural and gait abnormalities caused by hip-flexion deformity in spastic cerebral palsy: treatment by iliopsoas recession. For physeal fractures that do not attain this reduction tolerance, we advocate closed reduction under general anesthesia. Alternatively, a wedge of bone can be removed to accomplish a medial closing osteotomy. Tibial bowing (kyphosis) Achilles tenotomy Talus excision (Boyd) Carefully assess the position and shape of the talus and calcaneus to ensure abnormalities of the talus and calcaneus are known in advance. This directly exposes the superomedial fragment and keeps the neurovascular bundle in the anterior flap. Positioning the patient is placed in the standard supine position, and a general anesthetic is used in all cases. Subject to chronic and unremitting medial tension, there may be delayed or fragmented ossification of the medial malleolus.

